Oct 14, 2014
New Government
Ebola Hospital discharges 49 survivors after two weeks of operationThe Inspector-General of Police credited the onlooking President with encouraging them to think out of the box, which inspired him to offer the Hastings facility, as there was no police training ongoing. The Chief of Defence Staff, General S.O. Williams informed the audience that the Sierra Leone Military had made two army doctors available to the new facility.
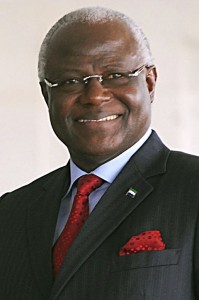 In
his address, President Koroma thanked the Ministry of Health for the
tremendous work they had done in establishing an Ebola Treatment Center
in so short a time and praised their efforts in curing so many
survivors. He called the exercise a great success and a showcase of our
national and collective efforts in the fight against Ebola. He said it
would show to the international community that
Sierra Leoneans themselves were making considerable effort and would
give them a stronger voice when negotiating with international
partners. He praised the efforts of all concerned, including the Sierra
Leone Police and military.
In
his address, President Koroma thanked the Ministry of Health for the
tremendous work they had done in establishing an Ebola Treatment Center
in so short a time and praised their efforts in curing so many
survivors. He called the exercise a great success and a showcase of our
national and collective efforts in the fight against Ebola. He said it
would show to the international community that
Sierra Leoneans themselves were making considerable effort and would
give them a stronger voice when negotiating with international
partners. He praised the efforts of all concerned, including the Sierra
Leone Police and military.We at natinpasadvantage would urge caution in the operations of the Hastings Ebola Center. It is certainly a highly laudable effort to help Sierra Leone by the Ministry of Health and the doctors, nurses and other health workers involved, but bitter experience with Ebola teaches us that the disease should never be underestimated. Every effort should be made not to compromise safety, even in the face of urgings for greater efforts from politicians and top ministry officials safely ensconced in remote, air-conditioned offices. International experts working with Ebola are extremely conservative in handling it because they know how dangerous it can be. The government-run Kenema Ebola Center ended in well-documented (see Are we repeating the Kenema mistake in Freetown?) disaster. MSF, with the most experience of any organisation in handling Ebola, ideally start their centers slowly and take considerable time training their staff. They are careful not to overextend their workers or subject them to fatigue, because they are well aware that fatigue encourages mistakes. They rotate international staff out of the country after a tour of some weeks.
MSF's Kailahun Case Management Center, operating since the start of the outbreak in May had admitted a total of 606 patients, with 391 confirmed Ebola cases in the four months to Sept. 24. Its new Ebola clinic in Bo, opened on the same date, Sept 19, as the Hastings Center, had admitted just 15 patients up to Sept 24. With 502 hospital beds in the West African region and somewhere between 2,239 and 3,058 health workers (depending on what category of staff are included) MSF has between 4 and 6 staff members per hospital bed (all sources MSF webpage Ebola ). The Hastings Ebola Center has less than 2 staff members per hospital bed. The Red Cross started its new center in Kenema (the replacement for the ill-fated Kenema government Ebola center) on September 12, with 80 local workers and 19 international staff caring for 21 patients (see New Ebola Treatment Center). They plan to slowly increase the number as they build up experience and train staff.
Under the most favourable conditions, in developed countries treating a single patient in climate controlled conditions with sophisticated equipment, ample staff and medical supplies and top-quality Personal Protective Equipment, we know that Ebola still manages to find a way to infect medical workers. It happened first in Spain, now in the United States. If this is possible in these countries, how much more likely is it here, given our conditions? Infection of health workers is one of the prime methods by which the virus spreads, and is to be avoided at all cost. We would urge a slow, careful, studied buildup of experience in Ebola treatment.
Editor's note: A week after this ceremony, and after our initial publication of this piece, the hospital discharged an additional 33 Ebola survivors.